A Global View of Wellness: Merging Ancient Systems with Modern AI
Perhaps the most intellectually captivating development in this landscape is the application of cutting-edge computational power to traditional, non-Western medical systems. For billions across the globe, systems like Ayurveda, Traditional Chinese Medicine, or various Indigenous healing practices are not relics; they are the primary source of healthcare, often utilized when Western biomedical models are inaccessible or culturally dissonant.
The World Health Organization (WHO), recognizing this global reality, has actively championed the use of AI to complement and enhance what is broadly termed Traditional, Complementary, and Integrative Medicine (TCIM). This is not about replacing ancient wisdom but about using modern tools to validate, catalog, and respect it.
Digitizing Heritage, Preserving Sovereignty
Consider the work being done in nations rich with this heritage. In India, for example, sophisticated AI tools are actively working to digitally catalogue, analyze, and cross-reference centuries of indigenous medical texts. This process achieves two vital goals simultaneously: it preserves invaluable cultural heritage from potential loss and, crucially, it makes that knowledge computationally accessible for research and synthesis.
Researchers are using machine learning models to rapidly analyze the complex phytochemical structures of medicinal plants. The goal? To scientifically understand their efficacy against modern ailments, from inflammatory diseases to, as seen in pilot studies in the Republic of Korea, even specific compounds for treating blood disorders. This analytical integration proves AI is adaptable beyond purely reductionist biomedical models, fostering a more holistic and globally informed approach to well-being.. Find out more about AI applications for continuous remote patient monitoring.
However, this integration is fraught with necessary ethical consideration. The global TCIM market is projected to approach nearly **$600 billion in 2025**, a huge economic driver. With that much value, the risk of exploitation—or “biopiracy”—is real. The WHO’s initiative stresses that any digital cataloging must be accompanied by proactive measures to safeguard Indigenous Data Sovereignty (IDSov).
Actionable Insight for Researchers and Developers:
- Participatory Design: Ensure that local and Indigenous communities are partners in the design and governance of any AI system that digitizes their traditional knowledge.
- Benefit Sharing: Establish clear, ethical frameworks for intellectual property and benefit-sharing *before* commercialization or widespread academic publication.
- Contextual Validation: Utilize AI to find correlations within the traditional system’s own context, rather than immediately forcing it into a Western-centric validation structure.
- TPLC Mindset: Plan for post-market surveillance; the FDA expects safety monitoring to be continuous.
- Subgroup Analysis: Rigorously test and report performance across defined patient subgroups (race, age, sex) to check for fairness gaps.
- Human Oversight: Regulators signal that clinicians must retain meaningful human oversight; AI should support, not supersede, final human judgment.
- Data Ethics: Establish clear protocols for data use and consent, particularly when dealing with non-Western or Indigenous datasets.
- Invest in Interoperability Middleware: AI tools are only as useful as the data they can access and the systems they can talk to. Focus capital expenditure on infrastructure that ensures your Electronic Health Records (EHRs), new sensor platforms, and AI engines can communicate *without* manual data transfer.
- Mandate “Model Cards” in Procurement: When purchasing new AI diagnostic or predictive tools, demand the vendor provide a “Model Card” (as encouraged by recent FDA draft guidance). This document must clearly detail the model’s architecture, the composition of its training data (including demographic representation), and its known limitations or performance disparities across subgroups.
- Establish an AI Review Board: Create a multidisciplinary committee—including clinicians, IT security, legal/compliance, and patient advocates—to vet any new AI system. Their mandate should be to proactively test for bias and workflow disruption before the tool goes live for patient interaction. This is essential for managing risk and building institutional trust in clinical AI governance.
- Prioritize Staff Digital Literacy: The best tool fails if the user doesn’t trust it or doesn’t know how to interpret its output. Implement mandatory training not just on *how to use* the interface, but on the fundamental principles of *how the AI works* and where its failure points might be.
- Expect Continuous Oversight: The era of one-and-done regulatory approval for adaptive software is passing. Plan for lifecycle monitoring.
- Data Diversity is Non-Negotiable: Biased data yields biased care. Demand transparency on training sets to mitigate health inequity.
- Holistic Integration is an Opportunity: Look beyond Western models to find validated, AI-enhanced paths to personalized care, while respecting data sovereignty.
This respectful, analytical partnership—where computational analysis serves to illuminate, rather than dominate, millennia of wisdom—is a hallmark of genuinely transformative healthcare expansion. It speaks to a broader move toward integrative medicine future, one that honors diverse approaches to wellness.
The Governance Tightrope: Navigating Ethics, Bias, and Regulatory Scrutiny in 2026
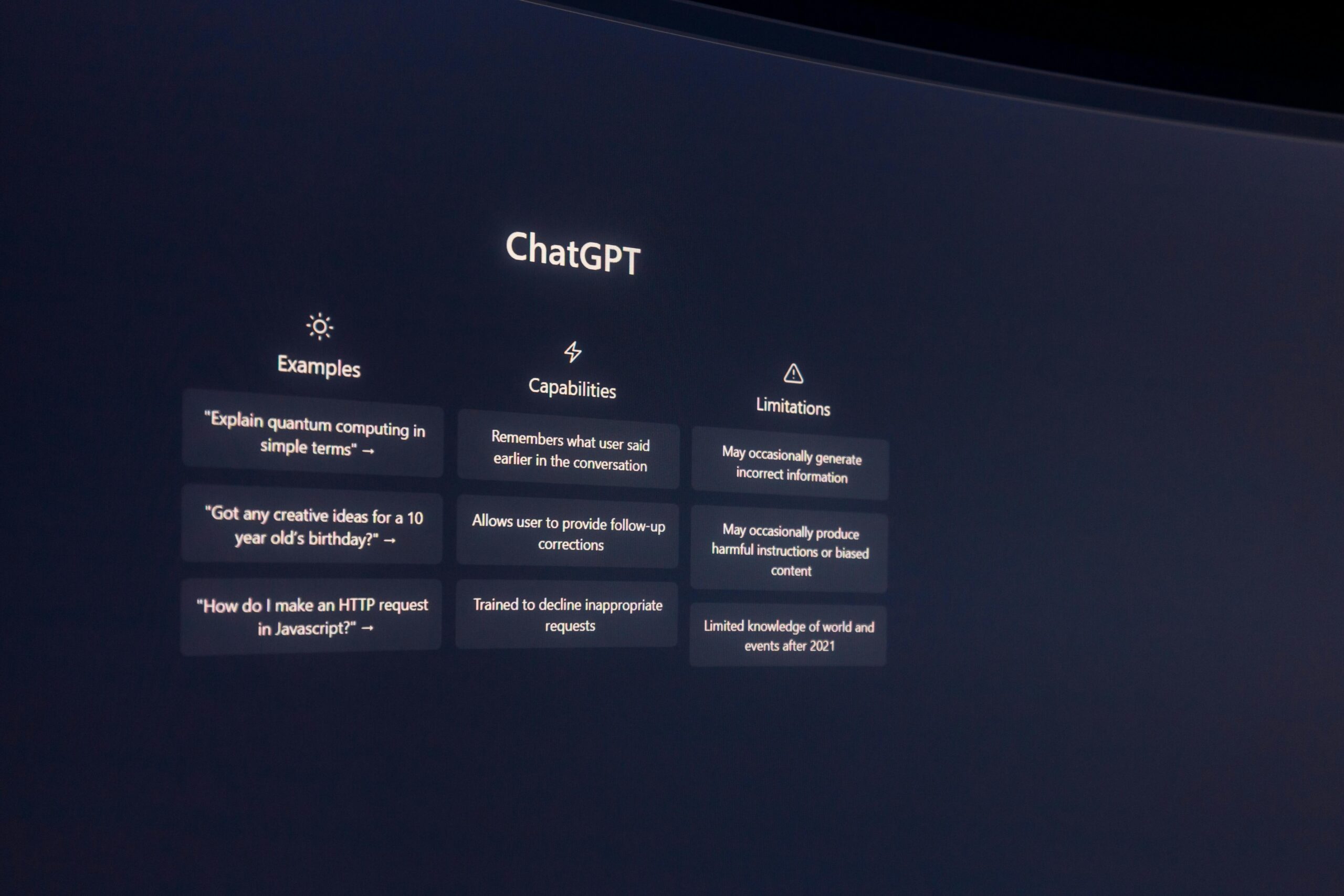
As AI embeds itself into life-and-death clinical pathways, the honeymoon phase for developers is officially over. The conversation has rightfully pivoted from “What *can* this AI do?” to “What *must* this AI do to be safe, fair, and accountable?” Innovation is now inextricably linked to responsibility, and in early 2026, the regulatory bodies are catching up with sharp, actionable guidance.
The core challenge is that the power of these tools demands an equivalent level of responsibility in their creation and deployment. As one recent analysis noted, AI in healthcare is triggering serious enforcement risks across HIPAA and FDA oversight, demanding stronger policies and patient consent practices. Healthcare organizations can no longer delegate their liability to an algorithm.
Establishing Frameworks for Algorithmic Fairness and Trust
The specter of algorithmic bias looms largest. If the datasets used to train a diagnostic model disproportionately feature data from, say, affluent, specific ethnic groups or exclude variations found in rural populations, the resulting model will perpetuate or even amplify existing health inequities. This isn’t just unfair; it leads to incorrect diagnoses and suboptimal treatment recommendations for underrepresented groups, sometimes with catastrophic consequences.
A chilling example surfaced from MIT research where AI models analyzing chest X-rays were highly accurate at predicting a patient’s self-reported race—a feat beyond human capability—but these same models exhibited the largest “fairness gaps,” meaning they were less clinically accurate for women and Black patients. This shows the danger: the model becomes too good at recognizing *who* the patient is based on data patterns, but too poor at treating *what* the patient has.. Find out more about AI applications for continuous remote patient monitoring tips.
To maintain the essential trust of clinicians and patients, transparency in building, validating, and implementing these AI applications is non-negotiable. There is a palpable demand for methodologies that allow medical teams to rigorously test AI systems on specific clinical tasks *before* patient deployment. This proactive stance on fairness is the dividing line between responsible progress and reckless adoption. To learn more about the strategies being employed to tackle this, look into recent literature on algorithmic fairness frameworks.
The Critical Role of Regulatory Oversight and Data Sovereignty
The technology continues to sprint, while regulation often walks. Agencies are actively grappling with how to govern software that is designed to *learn and change* over time—a concept far removed from the static, locked-down testing of a traditional Class II medical device.
In the United States, the Food and Drug Administration (FDA), under Commissioner Marty Makary, has signaled a significant pivot as of early January 2026. The agency has issued draft guidance pushing toward a Total Product Life Cycle (TPLC) approach for AI-enabled software functions, requiring continuous monitoring post-market, not just pre-market clearance. At the same time, the agency released new guidance around January 6, 2026, that appears to loosen regulatory burdens on certain Clinical Decision Support (CDS) software, betting that physician oversight can safely absorb faster deployment of tools that offer multiple recommendations rather than a single directive. Furthermore, updates in January 2026 have given broader leeway to wearables for general wellness claims, even for metrics like blood pressure, provided they are not intended for diagnosis or treatment.
This rapid evolution creates an environment where scientific rigor must meet regulatory agility. The challenge is complex, especially when considering data governance. As AI systems ingest massive amounts of sensitive personal health information, safeguarding that data becomes paramount. This is acutely felt in the context of digitized traditional knowledge, where proactive measures must be in place to prevent the exploitation of unique cultural or genetic information. Preserving Indigenous Data Sovereignty is a non-negotiable component of ethical deployment in these areas.
Key Regulatory & Ethical Checkpoints for 2026:. Find out more about AI applications for continuous remote patient monitoring strategies.
The Convergence: Building the Next-Generation Care Ecosystem
The true promise of this technological expansion isn’t found in any single development, but in the convergence of all these moving parts. Remote monitoring provides the *data*, AI provides the *analysis*, and the ethical/regulatory structures provide the *trust* to deploy it broadly. This collective effort paints a picture of a healthcare sector on the precipice of its most significant evolution yet.. Find out more about AI applications for continuous remote patient monitoring insights.
We are moving from episodic care, dictated by office hours and appointment availability, to a continuous, symbiotic partnership between human expertise and machine intelligence. This new ecosystem is being built on foundations that must be as sophisticated and adaptive as the technology itself.
Practical Steps to Engage with Continuous Care Models
For healthcare systems, administrators, and dedicated clinicians preparing for the next wave of integration, here are a few concrete areas to focus energy on, starting today:
The global push for better access, combined with technological capability, means that care is decentralizing. This requires a new level of organizational preparedness. We can no longer afford a reactive stance; the ethical and practical foundations being set in 2026 will determine the quality of medicine for decades to come.
Conclusion: Redefining Partnership in the Digital Age
The story unfolding in healthcare right now—centered on remote monitoring, computational synergy with global medical traditions, and a necessary reckoning with ethics—is easily the most important narrative in medicine this decade. The data is pouring in, promising a future where disease is intercepted, not just treated, and where care respects the full spectrum of human healing traditions.
The core of this transformation rests not on replacing the clinician, but on equipping them with superhuman insight. The AI in RPM market is growing because the utility is proven: it reduces hospital stays, empowers chronic disease management, and bridges geographical divides. The fusion with TCIM demonstrates a commitment to a truly global, multifaceted view of human health. And the intense focus on algorithmic fairness and adaptive regulation signals a maturing industry that understands high-stakes technology demands high-level responsibility.
Key Takeaways for Staying Ahead:. Find out more about Machine learning analysis of medicinal plant compounds insights information.
The next few years are critical. They will solidify whether this powerful partnership between human expertise and machine intelligence leads to a more equitable, precise, and humane healthcare system, or one riddled with unexamined bias and regulatory gaps. The interest across media outlets is well-justified; the decisions made now are building the very foundation of tomorrow’s patient experience.
What is your organization doing to move beyond *using* AI to *governing* AI? Are your current validation processes ready for the TPLC model, or are you still operating under the old clearance paradigm? Share your thoughts in the comments below!